The views expressed in this paper are those of the writer(s) and are not necessarily those of the ARJ Editor or Answers in Genesis.
Abstract
Until recently, human beings have long been considered sexually dimorphic, consisting of male and female sexes. This binary view of human sexuality is now being challenged by those who espouse an LGBTQ/transgender ideology. In the push to force acceptance of their beliefs on the public at large, transgender advocates claim there is a spectrum of human genders and that individuals can choose where they fall on that spectrum. They would also have us believe that individuals can change their sex via sex reassignment surgeries. These ideas are not based on biological realities. Biological sex is grounded in anatomy, physiology, and genetics. Here, I describe why—biologically—there are only two sexes (= genders) and why true sex reassignment is impossible.
Keywords: woman, man, gender, sex, sexuality, male, female, transgender
Introduction
On March 23, 2022, Supreme Court nominee Ketanji Brown Jackson testified before the Senate Judiciary Committee that she could not define a woman because she is not a biologist. While most people found it surprising that one must consult a professional biologist to define woman, it is true that biology can provide the answer. In this paper, I describe the biological basis of gender.
Sex versus Gender
Historically, gender and sex have been used interchangeably; that is, they are synonyms. Sex and gender are still seen as synonymous by some1 but recently viewed as distinct by others.2 To those who see them as distinct, gender may include behaviors, attitudes, feelings or other psychological or mental qualities. Consequently, they argue, there may be many (perhaps infinite) genders. Biologists must leave those arguments to the psychologists, sociologists, and others in those related behavioral sciences. From the perspective of biology (that is, anatomy, physiology, and genetics), the sexual distinction between male and female is unyielding to such psychological/social qualifiers; it is based on the anatomy of the genitalia, the genetics of the chromosomes, and the physiological processes of reproduction. Here, I continue to regard gender and sex as synonyms.
Anatomical Basis of Sex
Based on human anatomy (that is, structure), we find that there are two sexes called male and female. All non-anomalous human beings exist as one or the other and possess either the male or the female anatomical structures called genitalia. Males and females possess both external genitalia and internal genitalia. Males possess the anatomical structures identified as penis, testes, and scrotum, among others. Females possess the anatomical structures identified as vagina, uterus, and ovaries, among others. Excepting rare anomalies, all people possess either male genitalia or female genitalia.
Genetic Basis of Sex
The genitalia provide an anatomical definition of male and female. However, the genitalia are but outward expressions of the genetic blueprint present in every living cell in the human body. Deoxyribonucleic acid (DNA) stores this genetic information used to build the genitalia and all other parts of the body. In human cells, DNA is organized into 23 distinct chromosomes. Twenty-two of those chromosomes are called autosomes; the remaining chromosome is the sex chromosome, which directs sexual development. There are two versions of the sex chromosome (X and Y). In each human cell, there are two copies of each chromosome, that is, 23 chromosome pairs (46 chromosomes total). The sex chromosome pair may be either XX or XY; it is never YY. Thus, the sex chromosomes provide for the genetic definition of male (XY) and female (XX). Excepting genetic anomalies (see below), all people possess either the XX or XY sex chromosome pair.
Physiological Basis of Sex
Reproduction is the creation of a new individual from parent individuals. It is a physiological process. The biological purpose of having two sexes is reproduction with genetic mixing (as opposed to cloning). Mixing DNA from two individuals to create a genetically unique third individual spreads variation throughout a population. In humans, sexual reproduction employing the two sexes requires one of each sex. Two (or more) males cannot reproduce. Two (or more) females cannot reproduce. Only one male copulating with one female can reproduce.3 This observation is so basic and universal among mankind that most consider this fact self-evident.
As stated above, anatomy is the study of structure; it falls within the purview of descriptive science. Physiology is the study of function and falls within the purview of empirical science. Physiological processes can thus be studied by hypothesis and experiment and once understood can be manipulated. The physiological processes of reproduction include the production of gametes (sperm by male, ovum by female), the integration of one sperm with one ovum (fertilization), and the development of a subsequent offspring. These physiological processes naturally happen within the male and female internal genitalia, but technological advances are making it possible to perform several of these processes outside the human body, particularly fertilization and the later stages of fetal development. Understanding these processes has also allowed us to prevent pregnancy by manipulating the female reproductive cycle (for example, hormonal contraception). However, understanding these physiological processes has not allowed—and in principle cannot allow—the conversion of male to female, or vice versa.
Transgenderism and Sex Change
According to the online Cambridge Dictionary, transgenderism is “the condition of someone feeling that they are not the same gender (= sex) as the one they had or were said to have at birth.”4 The related gender dysphoria is the feeling of disconnection, discomfort, or distress surrounding the conflict between the gender with which one identifies and the gender assigned at birth.5 Dr. Paul R. McHugh, former psychiatrist-in-chief for Johns Hopkins Hospital, identified transgenderism as a mental disorder deserving compassionate treatment (rather than affirmation) and noted that any attempt at sex change is biologically impossible.6
Dr. McHugh is correct; it is biologically impossible to change one’s sex. Sex is not assigned by decree at birth by a parent or medical professional; it is assigned genetically at fertilization by the pairing of sex chromosomes (XX or XY). The genetic assignment is then expressed by the development of anatomical structures (that is, genitalia) and the initiation of physiological processes (for example, gamete production, menstruation, etc.). To conceivably convert a person genetically from one sex to the other, the DNA in every cell of the body must be altered from XX to XY (or vice versa). Anatomically, sex reassignment surgeries are available, but these only create imitations of real genitalia. For female-to-male (FTM) transformations, metoidioplasty converts the clitoris to a penis, but the penis it creates is too small for penetrative sex. Phalloplasty creates a penis from transplanted skin (usually the arm, thigh, or waist), but it is incapable of erection. Scrotoplasty produces a bag-like scrotum from the labia, but it is occupied by silicone implants, not functional testes. Likewise, for male-to-female (MTF) transformations the testes are removed but not replaced with functional ovaries. A faux vagina can be made (penile inversion vaginoplasty) and skin from the scrotum can be used to construct labia, but as with FTM, these transformations actually result in the mutilation of healthy body parts in exchange for anatomically subpar facsimiles of genitalia. To call these surgeries sex changes is to be biologically and medically dishonest. Physiologically, attempted FTM and MTF transitions require hormone therapy for years or life.
Genetic Anomalies
As noted above, there are 23 chromosomes in the human genome: 22 autosomes and 1 sex chromosome (either X or Y). In each human, these chromosomes exist as pairs, leading to 46 chromosomes total. The sex chromosome pair may be either XX (female) or XY (male). A visual sorting of the chromosomes from an individual is called a karyotype. The male and female karyotypes are shown in fig. 1. These 23 pairs of chromosomes are universally recognized as the normal chromosome arrangements in humans. Other arrangements exist, but they are derived from aberrant cell division and thus considered abnormal conditions (that is, anomalies).
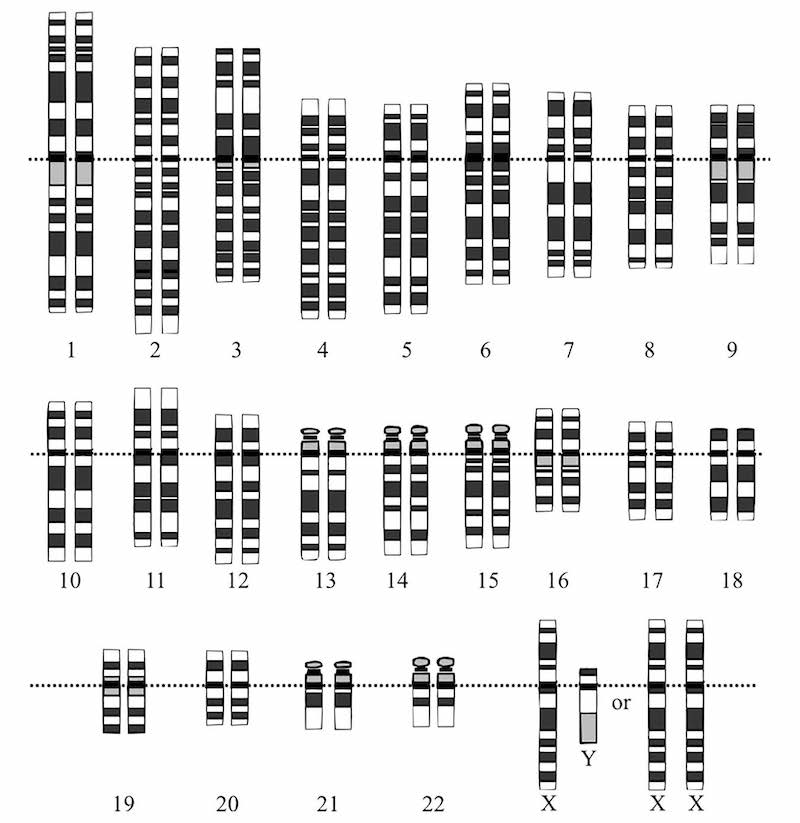
Fig. 1. Karyotype showing both male and female sex chromosomes. https://commons.wikimedia.org/wiki/File:Karyotype.png. Modified from Human Genome Project. Contributor: en:User:TedE.
In many circumstances, simply defining anomaly is tricky and subjective. Part of the problem lies in defining first what is normal. Thankfully, there is a well-defined normal in human genetics with respect to sex: XX = female, XY = male. The XX and XY chromosomal pairings are the normal patterns of inheritance regarding sex. Therefore, we can define a genetic anomaly with respect to the sexes as any genetic event producing something other than XX or XY for the sex chromosome. Most sex chromosome anomalies result in infertility, further confirming the anomalous (that is, abnormal) nature of these events.
Many anomalies with respect to genes and sex involve aneuploidy, the presence of an abnormally high number of chromosomes (that is, one or more additional chromosomes) making the total number larger than 46. Since there are normally two copies of each chromosome, having an extra copy of a chromosome is called trisomy. One extra copy of any autosomal chromosome is almost always lethal. The only autosomal trisomy that usually results in viability to adulthood is trisomy 21 (Down Syndrome) which causes cognitive and growth impairments and characteristic physical traits. Two or more extra copies of any autosome are always lethal.
Having additional copies of the sex chromosome is survivable. Some of the most common aneuploidies for the sex chromosome are listed in Table 1. The higher the chromosome number, the rarer the condition.
| 0 | X | XX | XXX | XXXX | XXXXX | |
|---|---|---|---|---|---|---|
| 0 | 00 (L) | X0 (F) | XX (F) | XXX (F) | XXXX (F) | XXXXX (F) |
| Y | 0Y (L) | XY (M) | XXY (M) | XXXY (M) | XXXXY (M) | |
| YY | YY (L) | XYY (M) | XXYY (M) | XXXYY (M) | ||
| YYY | YYY (L) | XYYY (M) |
Taking these survivable sex chromosome aneuploidies into consideration, the genetic definition of the sexes can be further refined: rather than XX being female and XY being male, anyone with a Y chromosome is defined as male.7 Thus, the mere presence of a Y chromosome defines male and the absence of a Y chromosome defines female.8 Since several sex chromosome aneuploidies are survivable, there are chromosomal variants of male and chromosomal variants of female (table 1), but all are either male or female. Viable male and female variants are described in table 2 and table 3, respectively.
| XYY syndrome | 1:1,000 | Few physical abnormalities; normal fertility |
| XXY (Klinefelter syndrome) | 1:1,000 | Few physical abnormalities; infertility |
| XXYY syndrome | 1:30,000 | Physical abnormalities & cognitive impairments; infertility |
| XXXY syndrome | 1:50,000 | Cognitive impairments; infertility |
| XXXXY syndrome | 1:100,000 | Physical abnormalities & cognitive impairments; infertility |
| X0 (Turner’s syndrome) | 1:2,500 | Distinct physical features; infertility |
| XXX syndrome (Trisomy X) | 1:1,000 | Slight physical or cognitive abnormalities; normal fertility |
| XXXX syndrome (Tetrasomy X) | <100 cases known | Symptoms range from mild (like XXX) to severe (like Pentasomy X) |
| XXXXX syndrome (Pentasomy X) | <40 cases known | Severe mental retardation & physical abnormalities |
Anatomical and Physiological Anomalies
As stated previously, anatomy is but a reflection of genetics. Males (XY) are genetically programmed to exhibit male genitalia and females (XX) are programmed to exhibit female genitalia. In rare instances, genetic mutations may disrupt this normal programming.
Complete Androgen Insensitivity Syndrome (CAIS)
CAIS (Complete Androgen Insensitivity Syndrome) is often cited as a deviation from the normal genetics-anatomy linkage. CAIS is presented by those who espouse LGBTQ/transgender ideology as a normal part of the spectrum of human variation in sexuality and gender. Indeed, one article on CAIS stated plainly that “lesbian, gay, and transgender individuals, from a biological perspective, represent some of the expected variation in sexual development” (Ness 2020). However, CAIS is not an expected variation; it is the result of a genetic mutation and is an exceedingly rare anomaly. (It is also illogical to conclude that homosexuality is an expected variation in sexual development since homosexuals cannot reproduce; reproduction being the raison d’être of biological sex).
Developmentally, one can consider the female sex as the default condition. The presence of the Y chromosome redirects development from female to male. CAIS is caused by a mutation in the androgen receptor gene, which is located on the X chromosome. The androgen receptor is required for normal developmental responses to testosterone; mutant forms of the protein do not respond to testosterone and, consequently, the cells, tissues, and organs that normally respond to testosterone do not. (This situation is somewhat analogous to type 2 diabetes where insulin is produced but not detected by cells of the body). The cells, tissues, and organs that would normally respond to testosterone default to the female condition and the expression (anatomically and physiologically) of primary and secondary male sexual characteristics are blunted. Without a functional androgen receptor, an individual that is genetically XY will develop female external genitalia. These individuals do not possess a uterus or ovaries, but they do possess testes (in the pelvis).
CAIS is usually detected following presentation of an inguinal hernia in premenstrual girls. The incidence of inguinal hernia in girls ages birth to 15 is 0.7% (Chang et al. 2016). Among girls presenting with inguinal hernias, about 1.5% exhibit CAIS (Sarpel, Palmer, and Dolgin 2005). Thus, CAIS afflicts only 0.01% of the female population. Still, assuming 150 million females in the United States, that amounts to roughly 15,000 women who are genetically XY.
CAIS represents a condition in which an individual is genetically male but develops anatomically (externally) as a female. Physiologically, these individuals are sterile and cannot reproduce. They do not appear to exhibit mental disorders or gender dysphoria due to CAIS; they identify as girls. While CAIS does present a unique biological ambiguity to sex, the condition is remarkably rare and is unambiguously an anomaly. That is, it does not represent the norm or even one point on a normal spectrum. Consequently, CAIS and similar anatomical anomalies are not considered valid arguments for accepting transgenderism as normal.
XX Male Syndrome
XX Male Syndrome is essentially the opposite of CAIS; an individual with an XX (female) chromosome pair develops anatomically as a male.
As stated previously, development as female is the default condition and the presence of the Y chromosome redirects development from female to male. A gene on the Y chromosome called SRY is largely responsible for this redirection. Indeed, SRY seems to be the master switch that diverts female development to male development (Kashimada and Koopman 2010).
During the production of gametes (sperm and egg), genes are randomly swapped between chromosome pairs. This gene-swapping increases phenotypic diversity in the population. Gene swapping occurs between each of the autosomal chromosome pairs and between the sex chromosome pair. When a man (XY) produces sperm, genes are randomly swapped between the sex chromosomes, in this case, between his X chromosome and his Y chromosome. After meiotic cell division, genetically unique sperm are created from these gene-swapping events. Those sperm can then be used to fertilize an egg.
During the gene-swapping events of the sex chromosome, the SRY gene remains (usually) with the Y chromosome but can be moved to the X chromosome. If a sperm with an SRY-containing X chromosome fertilizes an egg, the resulting embryo will be XX genetically (female), but the SRY gene will redirect development from female to male resulting in an XX individual with male anatomy. These individuals identify as male. Although they anatomically have a penis and testes, they are physiologically infertile. In some ways, XX Male Syndrome is akin to XXY Syndrome (Klinefelter syndrome) because one of the X chromosomes incorrectly contains genes belonging to the Y chromosome.
Conclusions
The Biology of Human Genders
Humans, like virtually all animals and plants on earth, exist as two sexes—male and female. Genetically, the two sexes are defined as having a Y chromosome (male) or lacking a Y chromosome (female). Adult humans are diploid and are sexually either XX (female) or XY (male). No YY combination is observed. On rare occasions, aneuploidy increases the number of sex chromosomes (for example, XXX or XXYY), but sex is still determined by the presence or absence of the Y chromosome. Aneuploid individuals that possess a Y chromosome present physically as males and those that do not present as females.
Anatomy is the outward expression of genetics. Certain genetic mutations thwart the anatomical expression of the Y chromosome in XY males (for example, CAIS) or inappropriately trigger male development in XX individuals (for example, XX Male Syndrome). However, these individuals appear anatomically as male if the trigger is activated (XX Male Syndrome) and female if it is not (CAIS).
CAIS and XX Male Syndrome represent conditions in which an individual is genetically one sex and anatomically (at least externally) the opposite sex. Physiologically, these individuals are infertile. They do not appear to exhibit mental disorders or gender dysphoria from the abnormality. While these conditions do present a unique biological ambiguity to sex, they are rare and unambiguously anomalies. That is, they do not represent the norm or points on a normal spectrum. Accordingly, CAIS, XX Male Syndrome, and similar genetic-anatomical anomalies are not considered valid arguments for accepting transgenderism as a “normal part of the spectrum of human variation in sexuality and gender” (Ness 2020). As biologists Colin Wright and Emma Hilton opined in a Wall Street Journal editorial in 2020: “In humans, reproductive anatomy is unambiguously male or female at birth over 99.98% of the time” (Wright and Hilton 2020). Rare exceptions do not abolish the rule but instead reinforce it. While sexual anomalies exist within the human population, these anomalies do not establish a spectrum of human sexuality. Human sexuality is binary, consisting of male and female.
In the first chapters of Genesis, we read of the creation of animals and mankind. Genesis 1:27 states plainly that God created humans male and female. In Genesis 7, the animals entered the Ark in pairs—male and female. The current trend to confuse people, especially adolescents, with respect to gender is nothing more than a spiritual attack designed to undermine biological and spiritual truths. As scientists, we need to hold the line on biological reality. As Christians, we must show love and render aid to those being victimized and damaged by this brand of spiritual warfare.
References
Chang, S.-J., J. Y.-C. Chen, C.-K. Hsu, F.-C. Chuang, and S. S.-D. Yang. 2016. “The Incidence of Inguinal Hernia and Associated Risk Factors of Incarceration in Pediatric Inguinal Hernia: A Nation-Wide Longitudinal Population-Based Study.” Hernia 20, no. 4 (August): 559–563.
Kashimada, Kenichi, and Peter Koopman. 2010. “Sry: The Master Switch in Mammalian Sex Determination.” Development 137, no. 23 (December): 3921–3930.
Ness, Bryan. 2020. “There is More to Human Sexuality Than XX and XY.” Spectrum, 5 February. https://spectrummagazine.org/news/2020/there-more-human-sexuality-xx-and-xy.
Sarpel, Umut, Shani K. Palmer, and Stephen E. Dolgin. 2005. “The Incidence of Complete Androgen Insensitivity in Girls with Inguinal Hernias and Assessment of Screening by Vaginal Length Measurement.” Journal of Pediatric Surgery 40, no. 1 (January): 133–136.
Wright, Colin M. and Emma N. Hilton. 2020. “The Dangerous Denial of Sex.” The Wall Street Journal, Opinion, February 13. https://www.wsj.com/articles/the-dangerous-denial-of-sex-11581638089?reflink=desktopwebshare_permalink.



